Prevalência de Distúrbios Respiratórios do Sono e Fatores Associados em Pacientes de um Centro de Atendimento Terciário
DOI:
https://doi.org/10.24265/horizmed.2025.v25n3.06Palavras-chave:
Keywords: Sleep-Wake Disorders; Risk Factors; Respiratory Disorders; Body Mass IndexResumo
Objective: To determine the prevalence of obstructive sleep apnea (OSA) confirmed by respiratory polygraphy and to analyze its association with sociodemographic, anthropometric, lifestyle, and comorbidity variables in patients attending a pulmonology outpatient clinic.
Materials and Methods: An observational, analytical, and retrospective study was conducted using medical records of adult patients evaluated for suspected OSA at the pulmonology department of Hospital de Especialidades No. 2 (IMSS) in Ciudad Obregón, Sonora, between January 2023 and December 2024. Patients who completed a respiratory polygraphy were included. Data collected included age, sex, weight, height, body mass index (BMI), neck and abdominal circumferences, physical activity and smoking habits, comorbidities, and place of origin. Descriptive statistics (central tendency and dispersion), frequencies, and percentages were calculated. The chi-square test was applied with statistical significance set at p ≤ 0.05.
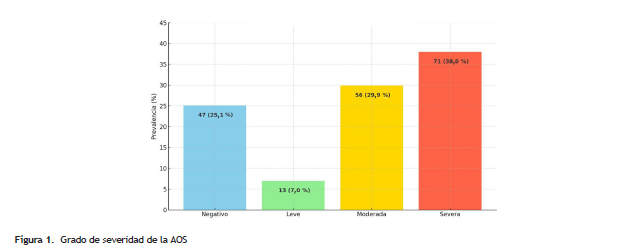
Results: Among 1,920 patients seen, 187 were evaluated for suspected OSA and 140 had a confirmed diagnosis, corresponding to a prevalence of 7.29%. The mean age was 53.1 years; the mean BMI was 33.7 kg/m², with obesity present in 55.1% of cases. The average neck and abdominal circumferences were 39.9 cm and 125.7 cm, respectively. Diabetes mellitus was present in 27.8%, isolated hypertension in 21.9%, and combined hypertension with other comorbidities in 12.3%. Only 31% engaged in regular physical activity, and 25.7% were smokers. Most patients originated from the municipalities of Cajeme and Guaymas.
Conclusion: OSA in our population is associated with middle age, central obesity, physical inactivity, and metabolic comorbidities. These findings underscore the importance of implementing systematic screening in pulmonology clinics, incorporating simple anthropometric measurements and risk factor assessments to improve diagnosis and guide multidisciplinary interventions.
Downloads
Referências
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Nunez C, Morrell MJ,
et al. Estimation of the global prevalence and burden of obstructive
sleep apnoea: a literature-based analysis. Lancet Respir Med.
;7(8):687–698. Disponible en: https://doi.org/10.1016/S2213-
(19)30198-5
Arnardottir ES, Mackiewicz M, Gislason T, Teff KL, Pack AI. Molecular
signatures of obstructive sleep apnea in adults: A review and
perspective. Sleep. 2009;32(4):447-70. Disponible en: https://doi.
org/10.1093/sleep/32.4.447
George CF. Reduction in motor vehicle collisions following treatment
of sleep apnoea with nasal CPAP. Thorax. 2001;56(7):508-512.
Disponible en: https://doi.org/10.1136/thx.56.7.508
Sharma SK, Agrawal S, Damodaran D, Sreenivas V, Kadhiravan
T, Lakshmy R, et al. CPAP for the metabolic syndrome in patients
with obstructive sleep apnea. N Engl J Med. 2011;365(24):2277-86.
Disponible en: https://doi.org/10.1056/NEJMoa1103944
Martínez-García MA, Capote F, Campos-Rodríguez F, Lloberes P, Díaz
De Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in
patients with obstructive sleep apnea and resistant hypertension:
The HIPARCO randomized clinical trial. JAMA. 2013;310(22):2407-15.
Disponible en: https://doi.org/10.1001/jama.2013.281250
Li X, Sotres-Alvarez D, Gallo LC, Ramos AR, Aviles-Santa L, Perreira KM,
et al. Associations of sleep-disordered breathing and insomnia with
incident hypertension and diabetes: The hispanic community health
study/study of latinos. Am J Respir Crit Care Med. 2021;203(3):356-
Disponible en: https://doi.org/10.1164/rccm.201912-2330OC
Lee W, Nagubadi S, Kryger MH, Mokhlesi B. Epidemiology of
obstructive sleep apnea: A population-based perspective. Expert
Rev Respir Med. 2008;2(3):349-364. Disponible en: https://doi.
org/10.1586/17476348.2.3.349
Redline S, Tishler P V., Hans MG, Tosteson TD, Strohl KP, Spry K.
Racial differences in sleep-disordered breathing in African-Americans
and Caucasians. Am J Respir Crit Care Med. 1997;155(1):186-92.
Disponible en: https://doi.org/10.1164/ajrccm.155.1.9001310
Jean-Louis G, Zizi F, Clark LT, Brown CD, McFarlane SI. Obstructive
sleep apnea and cardiovascular disease: Role of the metabolic
syndrome and its components. J Clin Sleep Med. 2008;4(3):261-72.
Disponible en: https://doi.org/10.5664/jcsm.27191
Kim J, Hakim F, Kheirandish-Gozal L, Gozal D. Inflammatory
pathways in children with insufficient or disordered sleep. Respir
Physiol Neurobiol. 2011;178(3):465-74. Disponible en: https://doi.
org/10.1016/j.resp.2011.04.024
Yang C, Zhou Y, Liu H, Xu P. The role of inflammation in cognitive
impairment of obstructive sleep apnea syndrome. Brain Sci.
;12(10):1303. Disponible en: https://doi.org/10.3390/
brainsci12101303
Epstein LJ, Kristo D, Strollo PJ, Friedman N, Malhotra A, Patil
SP, et al. Clinical guideline for the evaluation, management and
long-term care of obstructive sleep apnea in adults. J Clin Sleep
Med. 2009;5(3):263-76. Disponible en: https://doi.org/10.5664/
jcsm.27497
Mencar C, Gallo C, Mantero M, Tarsia P, Carpagnano GE, Foschino
Barbaro MP, et al. Application of machine learning to predict obstructive
sleep apnea syndrome severity. Health Informatics J. 2020;26(1):298-
Disponible en: https://doi.org/10.1177/1460458218824725
Chiu HY, Chen PY, Chuang LP, Chen NH, Tu YK, Hsieh YJ, et al.
Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP,
and Epworth sleepiness scale in detecting obstructive sleep apnea:
A bivariate meta-analysis. Sleep Med Rev. 2017;36:57-70. Disponible
en: https://doi.org/10.1016/j.smrv.2016.10.004
Montserrat JM, Sánchez-de-la Torre M, Terán J, Egea C. Los trastornos
respiratorios durante el sueño 2018: una nueva dimensión. Arch
Bronconeumol. 2019;55(3):122-123. Disponible en: https://doi.
org/10.1016/j.arbres.2018.05.012
Mitra AK, Bhuiyan AR, Jones EA. Association and risk factors for obstructive
sleep apnea and cardiovascular diseases: a systematic review. Diseases.
;9(4):88. Disponible en: https://doi.org/10.3390/diseases9040088
Thompson C, Legault J, Moullec G, Baltzan M, Cross N, Dang-Vu TT,
et al. A portrait of obstructive sleep apnea risk factors in 27,210
middle-aged and older adults in the Canadian Longitudinal Study
on Aging. Sci Rep. 2022;12(1): 5127. Disponible en: https://doi.
org/10.1038/s41598-022-08164-6
Genzor S, Prasko J, Mizera J, Kufa J, Zurkova M, Jakubec P, et al. Sex
transition from female to male as a risk factor for sleep-disordered
breathing. Sleep Med. 2023;102:180-185. Disponible en: https://doi.
org/10.1016/j.sleep.2023.01.006
Ahbab S, Ataoǧlu HE, Tuna M, Karasulu L, Çetin F, Temiz LÜ, et al.
Neck circumference, metabolic syndrome and obstructive sleep
apnea syndrome; Evaluation of possible linkage. Med Sci Monit.
;19:111-7. Disponible en: https://doi.org/10.12659/MSM.883776
Simou E, Britton J, Leonardi-Bee J. Alcohol and the risk of sleep apnoea:
a systematic review and meta-analysis. Sleep Med. 2018;42:38-46.
Disponible en: https://doi.org/10.1016/j.sleep.2017.12.005
Liu K, Zang C, Wang J, Liu J, Chen Z, He M, et al. Effects of common
lifestyle factors on obstructive sleep apnea: precautions in daily life
based on causal inferences. Front Public Health. 2024;12: 1264082.
Disponible en: https://doi.org/10.3389/fpubh.2024.1264082
Liu Y, Yang L, Stampfer MJ, Redline S, Tworoger SS, Huang T. Physical
activity, sedentary behavior, and incidence of obstructive sleep apnea
in three prospective US cohorts. Eur Respir J. 2022;59(2):2100606.
Disponible en: https://doi.org/10.1183/13993003.00606-2021
Khokhrina A, Andreeva E, Degryse JM. A systematic review on the
association of sleep-disordered breathing with cardiovascular pathology
in adults. NPJ Prim Care Respir Med. 2022;32(1):41. Disponible en:
https://doi.org/10.1038/s41533-022-00307-6
Yayan J, Rasche K. A systematic review of risk factors for sleep
apnea. Prev Med Rep. 2024;42:102750. Disponible en: https://doi.
org/10.1016/j.pmedr.2024.102750
Lo S, Mbanze I, Orr JE, DeYoung P, Checkoway H, Govo V, et al.
The prevalence of sleep-disordered breathing and associated risk
factors in patients with decompensated congestive heart failure in
Mozambique. J Clin Sleep Med. 2023;19(6):1103-1110. Disponible en:
https://doi.org/10.5664/jcsm.10510
Qian Y, Dharmage SC, Hamilton GS, Lodge CJ, Lowe AJ, Zhang J, et
al. Longitudinal risk factors for obstructive sleep apnea: A systematic
review. Sleep Med Rev. 2023;71:101838. Disponible en: https://doi.
org/10.1016/j.smrv.2023.101838
Huang Y, Xu J, Zheng S, Xu S, Wang Y, Du J, et al. The risk factors
for insomnia and sleep-disordered breathing in military communities:
A meta-analysis. PLoS One. 2021;16(5). Disponible en: https://doi.
org/10.1371/journal.pone.0250779
Erman MK, Stewart D, Einhorn D, Gordon N, Casal E. Validation of
the ApneaLinkTM for the screening of sleep apnea: A novel and simple
single-channel recording device. J Clin Sleep Med. 2007;3(4):387-92.
Disponible en: https://doi.org/10.5664/jcsm.26861
Stehling F, Keull J, Olivier M, Große-Onnebrink J, Mellies U, Stuck
BA. Validation of the screening tool ApneaLink® in comparison
to polysomnography for the diagnosis of sleep-disordered breathing in
children and adolescents. J Clin Sleep Med. 2017;37:13-8. Disponible
en: https://doi.org/10.1016/j.sleep.2017.05.018
Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, et
al. The AASM Manual for the Scoring of Sleep and Associated Events:
Rules, Terminology and Technical Specifications. Version 2.4. Darien
(IL): American Academy of Sleep Medicine; 2017. Disponible en:
https://pulmo-ua.com/wp-content/uploads/2021/12/AASM-sleepscoring-
Ben-Noun LL, Sohar E, Laor A. Neck circumference as a simple
screening measure for identifying overweight and obese patients.
Obes Res. 2001;9(8):470-7. Disponible en: https://doi.org/10.1038/
oby.2001.61
World Health Organization. Waist circumference and waist-hip ratio:
report of a WHO expert consultation, Geneva, 8–11 December 2008.
Geneva: World Health Organization; 2011. Disponible en: https://iris.
who.int/handle/10665/44583
Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl
:S31-S34. Disponible en: https://doi.org/10.4103/sja.SJA_543_18
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased
prevalence of sleep-disordered breathing in adults. Am J Epidemiol.
;177(9):1006-14. Disponible en: https://doi.org/10.1093/aje/
kws342
Deng X, Gu W, Li Y, Liu M, Li Y, Gao X. Age-group-specific associations
between the severity of obstructive sleep apnea and relevant risk
factors in male and female patients. PLoS One. 2014;9(9). Disponible
en: https://doi.org/10.1371/journal.pone.0107380
Pinto JA, Godoy LBM, Marquis VWPB, Sonego TB, Leal CFA, Ártico
MS. Anthropometric data as predictors of obstructive sleep apnea
severity. Braz J Otorhinolaryngol. 2011;77(4):516-521. Disponible en:
https://doi.org/10.1590/S1808-86942011000400017
Tian H, Wang A, Wu H, Zhou C, Zhang Z, Wang J. The causality
between leisure sedentary behaviors, physical activity and obstructive
sleep apnea: a bidirectional Mendelian randomization study. Front
Public Health. 2024;12. Disponible en: https://doi.org/10.3389/
fpubh.2024.1425060
Unal Y, Ozturk DA, Tosun K, Kutlu G. Association between obstructive
sleep apnea syndrome and waist-to-height ratio. Sleep Breath.
;23(2):523-9. Disponible en: https://doi.org/10.1007/s11325-
-1725-4
Halima KM, El-Daboosy AM, Awad S, Abo Al-Hassan A, Nour MO. Body
mass index as a predictor for obstructive sleep apnea in snoring
patients. Al-Azhar Med J. 2021;50(4):3123–36. Disponible en: https://
doi.org/10.21608/amj.2021.196451
Pinto JA, Ribeiro DK, Da Silva Cavallini AF, Duarte C, Freitas
GS. Comorbidities associated with obstructive sleep apnea: A
retrospective study. Int Arch Otorhinolaryngo.2016;20(2):145-50.
Disponible en: https://doi.org/10.1055/s-0036-1579546
Asad F, Moin M, Ubedullah, Rehman SU, Rehman FU. Relationship of
neck circumference and obstructive sleep apnea: a cross-sectional
study in Pakistani population. J Pharm Res Int. 2022;34(44A):47–53.
Disponible en: https://doi.org/10.9734/jpri/2022/v34i44A36333
Young T, Skatrud J, Peppard PE. Risk factors for obstructive sleep
apnea in adults. JAMA. 2004;291(16):2013-6. Disponible en: https://
doi.org/10.1001/jama.291.16.2013
Nasser J, Habib F, Malallah F, Darwish N, Rabie E. Risk for obstructive
sleep apnea among people with diabetes. Bahrain Med Bull. 2014;36(3).
Disponible en: https://doi.org/10.12816/0008106
Vana KD, Silva GE, Carreon JD, Quan SF. Using anthropometric
measures to screen for obstructive sleep apnea in the Sleep Heart
Health Study cohort. J Clin Sleep Med. 2021;17(8):1635-1643.
Disponible en: https://doi.org/10.5664/jcsm.9268
Downloads
Publicado
Como Citar
Edição
Seção
Licença
Copyright (c) 2025 Horizonte Médico (Lima)

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.
Os resultados de pesquisa da revista Horizonte Médico (Lima) (Horiz. Med.) são publicados sem custo e estão disponíveis gratuitamente para download sob o modelo de acesso aberto, com o objetivo de disseminar trabalhos e experiências desenvolvidos nas áreas biomédica e de saúde pública, tanto nacional quanto internacionalmente, e promover a pesquisa nos diferentes campos da medicina humana. Todos os manuscritos aceitos e publicados na revista são distribuídos gratuitamente sob os termos de uma licença Creative Commons - Atribuição 4.0 Internacional (CC BY 4.0).